If you’ve ever been behind the scenes at a clinic or hospital, you know one thing for sure: billing isn’t simple. Every day, staff are buried under insurance claims, complex codes, mountains of patient records, and strict regulations. It can get overwhelming, fast.
That’s why automated medical billing systems are becoming more common. For healthcare providers keeping up with paperwork is a big struggle, and automation helps bring order to the chaos.
Recent research shows just how important these systems have become. The medical billing software market is estimated to reach $17.92 billion in 2024, with expectations to grow to $32.18 billion by 2030. This means the industry is growing at an average rate of 10.2% per year, according to The Research Insights.
One of the slowest parts of the process is entering codes, submitting insurance claims, and adding in demographic information. Mistakes here are pretty common, from typing errors to using the wrong medical codes.
What You’ll Learn in This Guide
I’ll explain:
-
What an automated medical billing system is
-
Why these systems are valuable
-
Key features you should look for
-
How to create a system like this
-
And what pitfalls to avoid along the way
What Is Medical Billing Automation?
Medical billing automation uses computer software to handle day-to-day billing tasks quickly and with fewer mistakes. When a healthcare organization needs to submit insurance claims, this type of software can manage key steps like cleaning up claims, entering charges, and handling payments automatically—sometimes using timers and artificial intelligence tools like natural language processing to read and process information fast.
Here’s how it works in a bit more detail:
- Routine Tasks Are Done Instantly: Instead of someone manually entering every piece of data, the system fills in most fields, checks for errors, and sends claims electronically to insurance companies. It takes in information about the patient, the care given, and insurance details, and prepares the required forms and billing codes.
- Claims Are Scrubbed and Sent: Before a claim is sent, the software checks for mistakes or missing codes. If it finds issues, it flags them so they can be fixed right away. This helps claims get approved on the first try, which speeds up the time it takes to get paid.
- Payments and Remittance Handled Fast: When payments come in from insurance or patients, the software matches them to the correct account and marks the bill as paid or partially paid. It can also send out reminders for overdue payments or generate regular statements for patients.
- Less Manual Work, Fewer Errors: Because there’s little manual typing or copying and pasting, billing errors drop dramatically. The computer program remembers each step, catches issues, and follows up without getting tired or distracted.
- Improved Income and Profits: Automating billing means clinics and hospitals get paid faster and spend less time fixing mistakes. Over time, this raises income and helps the organization be more profitable—all while giving staff more time to focus on patients instead of chasing paperwork.
Why Is Automation Required For The Medical Billing Systems?
Automation handles every significant medical billing component that a person might find monotonous. Artificial intelligence can improves this process further by detecting errors before claims are submitted, making the entire system faster and more reliable.
Beyond robotic process automation (RPA) that handles tasks like sending text or email bill reminders to patients, AI can analyze patient communication patterns to optimize the timing and content of these messages, helping increase collections.
Given the large amounts spent annually on healthcare in the US alone, AI-driven improvements in billing accuracy and efficiency can reduce costly mistakes, speed up reimbursements, and lower administrative overhead for providers.
Let's dig deep into the importance of a billing system.
1) AFFORDABLE PRICES
RCM is the process of obtaining payments for medical bills to bring in money for the healthcare sector. Because it combines administrative data like personal information of a patient, treatment codes, insurer name, etc., making the management time-consuming and expensive.
Implementing an automated medical billing system increases your business cash flow and frees up time and resources, helping you concentrate on patient-focused tasks.
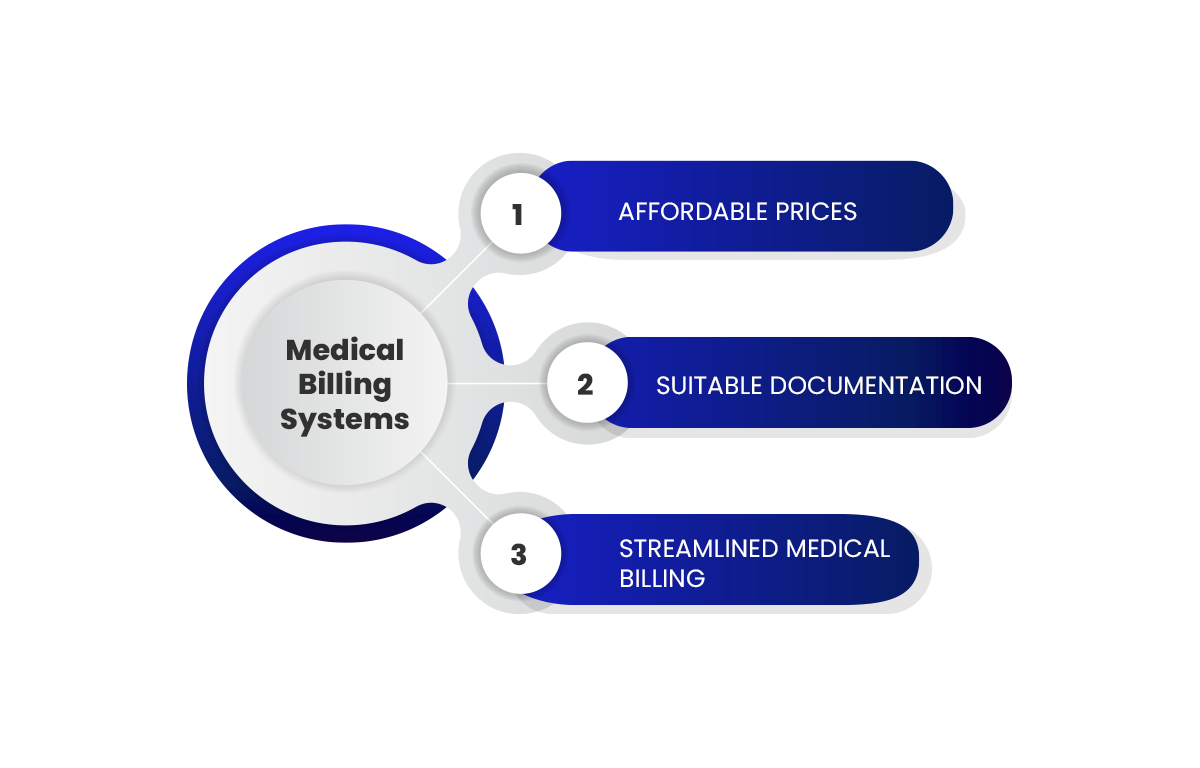
2) SUITABLE DOCUMENTATION
In this era, a single filing of a paper document costs $20 for a procedure, and then you must access the cost, and employees are required to fill out about 20,000 forms every year. Thus, medical billing involves a significant amount of administrative paperwork, such as creating and registering patient profiles, eligibility checks, and other validation, as error-free documentation is the aim of every healthcare provider.
Ergo, using Automation in medical billing boosts productivity while cutting down on the number of employees assigned to specific processes.
3) STREAMLINED MEDICAL BILLING
An outdated billing system brings disorganized claims and unnecessary errors, as per healthcare providers. For example, as per the Centers for Medicare & Medicaid Services, coding errors cost $28.91 billion in payment errors in 2019.
Also Read: RPA Use Cases In Payroll Management
What Role Does Medical Billing Automation Play?
Automation covers many tedious aspects of medical billing. When augmented with artificial intelligence, it takes a further step by using predictive analytics to evaluate claims before submission. By analyzing past claim outcomes and recognizing data patterns, AI estimates the likelihood that a claim will be approved or if it faces potential delays in payment. This allows billing teams to prioritize follow-ups on high-risk claims and reduce waiting times for reimbursements.
In addition to forecasting approvals, AI systems scan claims for unusual activity that may indicate fraudulent behavior. These systems spot irregular trends such as repeated billing for the same service or inconsistent coding practices. By catching such discrepancies early, providers can address issues promptly, minimizing financial losses caused by fraud.
The combination of predictive insights and fraud detection helps maintain accuracy and integrity throughout the billing process.
This proactive approach improves cash flow predictability and reduces the administrative burden of dealing with denials or underpayments, freeing personnel to focus on more complex cases and patient care.
Curious about our work in healthcare app and EHR development?
See how Zenesys has helped healthcare providers build smart, secure, and scalable digital solutions to streamline patient care and operations.
Explore Our Healthcare ProjectsWhat Is the Medical Billing System Automated with?
1) INSURANCE
The most significant step in an automated medical billing process is insurance. To gather data, such as entries from patients' medical histories, insurance eligibility, and drug and disease codes, healthcare professionals must sort with the help of different insurance systems. Based on the accuracy of the medical billing codes, then the payment is made.
2) HIPAA COMPLIANCE
Healthcare organizations must embrace Automation and integrate RPA development services to reduce security risks, maintain HIPAA compliance, and foster a successful relationship between doctor and patient. Most procedures for filling information approved by patients reduce the scope of omissions and errors.
These typically result in skipping steps and making the most basic mistakes. However, properly implementing RPA encourages Automation in healthcare workflow to assist with the automatic transfer of patient data.

3) APPOINTMENTS AND SCHEDULING
When RPA bots sort appointments and registrations from the start of consultation until it is over, the appointment and scheduling automation can easily streamline the scheduling process for patients.
4) MONITORING CLAIMS
Automating claims processing can ensure accurate payments so that no claim goes unpaid or is underpaid. By utilizing RPA in claim processing, your business can avoid any loss that might arise from underpayments.
Step-by-step Guide To Implement RPA Automation In Medical Billing
1) REGISTRATION
A patient must pre-register for a doctor's appointment by providing insurance information. Old appointment information will already be saved, so patients only need to give their visit's purpose when they return. Before submitting a claim, registered medical billers can check the information provided.
2) CHECK YOUR FINANCIAL RESPONSIBILITY
Financial responsibility investigations are conducted to confirm patient insurance to determine who is responsible for what for a doctor's visit. A biller must first gather crucial data, which can only be done by conducting financial responsibility checks to ascertain whether a patient's insurance plan covers the services the patient requires.
Since every person and business has a different insurance policy, a biller must confirm the patient's coverage before assigning any bills and ensuring that prescriptions are fully covered. In this instance, these checks are performed by RPA bots.
3) BOOKINGS
To distinguish between registered and first-timers, patients are asked to complete when they arrive. For example, whether copayments are received before or after the enrollment is completed by providing official identification, such as a valid insurance card and a passport or driver's license.
Copayments are typically collected at the point of service, and after the patient's identity has been confirmed, a report is sent to the medical coder. The medical coder examines the medical report after receiving it and converts the data into useful medical code. The "superbill" is the end product of the medical coding process.
The superbill contains demographic data regarding the patient's medical background, the doctor's and provider's names, the codes for the diagnosis and procedure, the procedures carried out, and other pertinent medical data. The superbill is then sent to the medical biller via software.
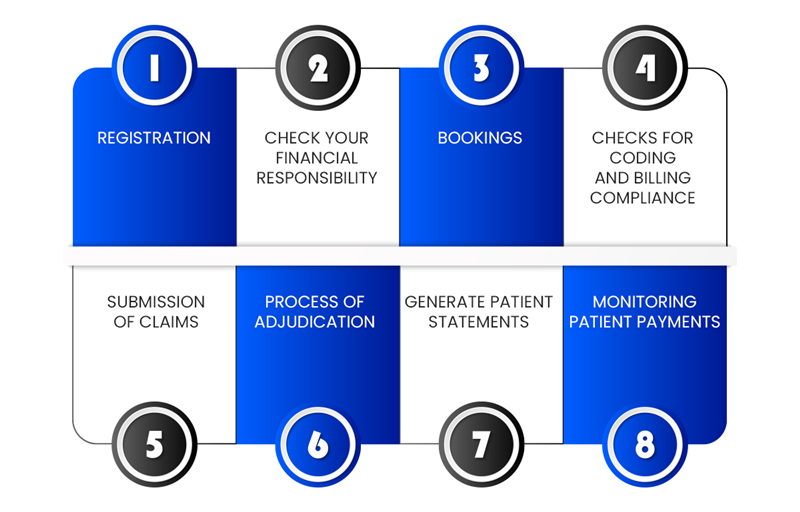
4) CHECKS FOR CODING AND BILLING COMPLIANCE
Although the billability of a procedure largely depends on the rules established by the payer and the patient's insurance plan, the medical biller ensures that the procedures coded are billable after receiving the superbill and transferring it into billing software or a paper claim form.
Standards for compliance must also be met, according to billers. For example, the Health Insurance Portability and Accountability Act and Office of Inspector General (OIG) compliance standards typically require the code to adhere to certain rules (HIPAA).
5) SUBMISSION OF CLAIMS
Through EDI, claims are transmitted electronically and with coding (Electronic Data Interchange). All healthcare organizations subject to HIPAA must submit their claims electronically under the Health Insurance Portability and Accountability Act of 1996 (HIPAA). Claims, however, will only be sent via EDI if they are error-free.
6) PROCESS OF ADJUDICATION
At this point, a claim is either accepted, rejected or denied. A payer assesses a medical claim to determine whether it is valid or compliant and the amount that will be paid to the provider. The biller or provider is sent the details of the claims during the adjudication process so they can determine how much they are willing to pay and why.
After the primary insurer has approved the claim for patients with secondary insurance, the remaining amount is sent to the secondary insurer. If there is a problem, the payer may initiate an appeal process.
7) GENERATE PATIENT STATEMENTS
The care that the patient has received from their healthcare provider is described in detail in patient statements. Once the payer has paid the agreed-upon sum, the patient is responsible for the remaining balance. To explain why some procedures were covered, and others weren't, some payers may include an Explanation of Benefits (EOB).
8) MONITORING PATIENT PAYMENTS
Paying bills on time is necessary to keep a system running smoothly. To ensure that medical bills are paid on time, billers are responsible for mailing out precise, timely bills.
When it comes to bill payments, notifications, and collections, they have their own set of policies and deadlines. If the patient does not pay the full amount or is past due, the biller must ensure that the provider is fairly compensated for their services.
Here are the key pitfalls to avoid
Automating medical billing can save time, reduce errors, and boost revenue—but only if it’s done right. While the benefits are real, there are a few common pitfalls that healthcare providers should watch out for during implementation and daily use.
Here are the key pitfalls to avoid:
- Choosing the Wrong Software: Not all billing software is created equal. Some systems might lack necessary features like claim scrubbing, real-time reporting, or EHR integration. Before committing, providers should ensure the solution aligns with their specialty, practice size, and workflow needs.
- Skipping Staff Training: Automation doesn’t mean you can skip human involvement. If the staff isn’t properly trained to use the system, errors can still occur. Invest time in onboarding, continuous training, and support to get the most out of your tools.
- Failing to Customize Workflow: Many billing tools allow customization—like setting rules for claim validation, auto-generating reports, or creating alerts for denied claims. Relying on default settings without tailoring them to your practice may lead to inefficiencies or missed opportunities.
- Ignoring Compliance and Security: HIPAA and other healthcare regulations require strict handling of patient data. Some practices overlook encryption, access control, or audit logs when setting up their billing software. Always verify that the system complies with industry standards and keeps data secure.
- Relying Too Much on Automation: While software can handle most billing tasks, it’s not foolproof. There still needs to be human oversight to review high-value claims, investigate denials, and ensure complex coding is done correctly. Automation should support—not replace—your billing team.
- Not Updating Coding Rules: Medical codes (like ICD and CPT) frequently change. If your software isn’t updated with the latest rules, claims may get rejected. Always ensure that updates are applied regularly or choose software that updates coding libraries automatically.
- Overlooking Patient Communication: Automated systems can send reminders and statements, but if these aren’t clearly written or timed well, patients may ignore them. Customize communication templates and schedules to improve engagement and payment rates.
- Neglecting Regular System Audits: Once automation is in place, some clinics forget to check how well it’s working. Conduct periodic audits to catch gaps, review denied claims, and fine-tune system performance. This ensures your setup stays accurate and efficient over time.
Avoiding these pitfalls helps ensure your billing automation project doesn't just work—but works well. It’s about striking the right balance between technology and human expertise, so your practice can run smoother and get paid faster without unnecessary setbacks.
Looking to automate your medical billing and cut down on claim errors?
Let Zenesys help you build a custom medical billing solution that's fast, secure, and built for healthcare professionals.
Get Your Custom SolutionHow Zenesys Can Help with AI-Driven Medical Billing Automation
Or we can implement predictive analytics to forecast which claims may face delays or denials, allowing billing teams to focus on high-priority cases and improve cash flow. Our AI-powered fraud detection tools scan billing patterns to spot irregularities early, helping minimize financial losses.
We also integrate robotic process automation alongside AI to handle routine tasks like claims submission, payment matching, and sending patient reminders. This combination frees up staff to concentrate on exceptions and patient care.
Whether it’s ensuring HIPAA compliance or customizing workflows specific to your practice, Zenesys works closely with healthcare providers to deliver secure, precise, and adaptable billing solutions that fit unique needs.
Wrapping Up
If your software is outdated, you risk dealing with a lengthier claim, processing times, non-payments, incorrect codes, disconnections with current billing codes, and a decline in profit. Medical Billing Automation is crucial for the business revenue cycle and makes the medical facility most effective and efficient.
Automation benefits a wide range of people, including patients and employees because it makes repetitive processes simpler and error-free, including medical billing, claims, scheduling, and more.
Thus, having a relaxed work environment is possible if you opt for a streamlined and optimized workflow. You can reduce human error and accurate the process using automated medical billing procedures.


.webp?lang=en-US&ext=.webp)

.webp?lang=en-US&ext=.webp)