And yet demands keep rising.
Costs are climbing. Chronic illnesses are spreading. Populations are aging.
The system isn’t built to handle this scale. Human effort alone simply can’t keep up.
That’s where the urgency comes in. Artificial Intelligence isn’t a nice-to-have idea. It’s already proving to be the difference between care that saves lives and care that collapses under its own weight.
AI is not about hype. It’s about fixing real cracks in the system—errors, inefficiencies, and lives lost due to delays.
And the organizations that act now? They’ll save money, save time, and above all, save patients.
In this article, we’ll dig into the use cases, applications, benefits, and solutions for AI in healthcare. We’ll also talk about AI agents, governance, and what it takes to move from pilot projects to real-world impact.
Key Takeaways (Facts that Matter)
- According to a report, the global AI in healthcare market size is expected to reach USD 187.69 billion by 2030, registering a CAGR of 38.62% from 2025 to 2030.
- Studies show 48% of healthcare executives already use AI in select areas, but only 6% use it at scale. That gap is where opportunity lives.
- 50% of AI-based medical devices approved in the US and Europe are for radiology, with AI systems outperforming radiologists in detecting conditions like pneumonia from chest X-rays.
- Admin work consumes almost 40% of a doctor’s working hours. AI-driven RPA can cut this time in half.
- 94% of healthcare organizations see AI as core to their operations, and 86% are currently using AI extensively.
(Source: Blue Prism Global Enterprise AI Survey 2025)
The biggest benefit? AI gives doctors back time—and patients back attention.
What Exactly Is AI in Healthcare?
AI in healthcare refers to computer systems that can analyze data, recognize patterns, and assist humans in making decisions.
Think of it as a digital assistant that never sleeps, never forgets, and can process thousands of cases faster than any human could.
Here’s where it shows up:
- Algorithms that scan X-rays for early signs of cancer.
- Virtual health assistants answering patient questions 24/7.
- AI agents that predict patient readmissions before they happen.
- Automation tools that cut down paperwork for staff.
It’s not about replacing doctors. It’s about giving them better tools to care for patients.
Why This Matters More Than Ever
If you ask a doctor today what burns them out most, it won’t always be patients. It’s the paperwork.
This is particularly true for mental health professionals, where the use of the best therapy note AI tools is becoming a game-changer for reducing administrative burden. Billing codes. Insurance rejections. Prescription management. Digital forms. Endless EHR clicks.
The cruel twist?
Patients lose out. Doctors spend only about 12 minutes on average per consultation in the US. And nearly half that time is glued to a screen, updating records.
AI can flip that balance. It can take the admin weight, process records faster, and free doctors to do the one thing only humans can: connect with people.
Sounds obvious, right? But here’s what most administrators miss when they think about AI:
This isn’t about replacing staff. It’s about re-engineering the workflows that break staff.
Without AI, hospitals risk drowning in endless tasks, errors, and wait times. With AI, they can redesign for speed, safety, and satisfaction.
AI promises something different:
- Quicker diagnosis.
- Shorter wait times.
- Lower costs.
- More time for doctors to focus on people instead of paperwork.
What are the Use Cases of AI in Healthcare?
When people talk about “AI in healthcare,” some picture robots doing surgery. That’s cartoon thinking. The reality is more practical—and already saving both money and lives.
Let’s break down the solutions AI is delivering right now:
1. Predictive Analytics and Forecasting
Imagine if hospitals could see next week’s bed demand before it happens. AI models already do this. They track local flu trends. They forecast ICU needs. They predict when supplies will run short.
During COVID-19, predictive AI tools helped states in the US anticipate ICU shortages days before they happened, letting them redirect ventilators in time.
2. Medical Imaging and Diagnostics
AI doesn’t get tired at 3 a.m. It reads scans the same way, every time, with consistent focus.
According to a recent survey-based study, an AI system trained on 288,767 exams and over 5.4 million breast ultrasound images achieved an AUROC of 0.976 on a test set of 44,755 exams. The AI outperformed an average of ten board-certified breast radiologists, who scored an AUROC of 0.924 ± 0.02, with the AI scoring 0.962.
Importantly, when used alongside radiologists, the AI helped reduce false positive rates by 37.3% and cut the number of biopsies requested by 27.8%, all while maintaining the same sensitivity level.
These results highlight the potential of AI to improve breast ultrasound diagnosis accuracy and reduce unnecessary procedures. AI also helps improve radiology turnaround time benchmarks, speeding up the review and reporting of diagnostic images, so patients get results faster and radiologists can focus on more complex cases.
Doctors don’t lose authority here. They gain a second set of eyes that never blinks.
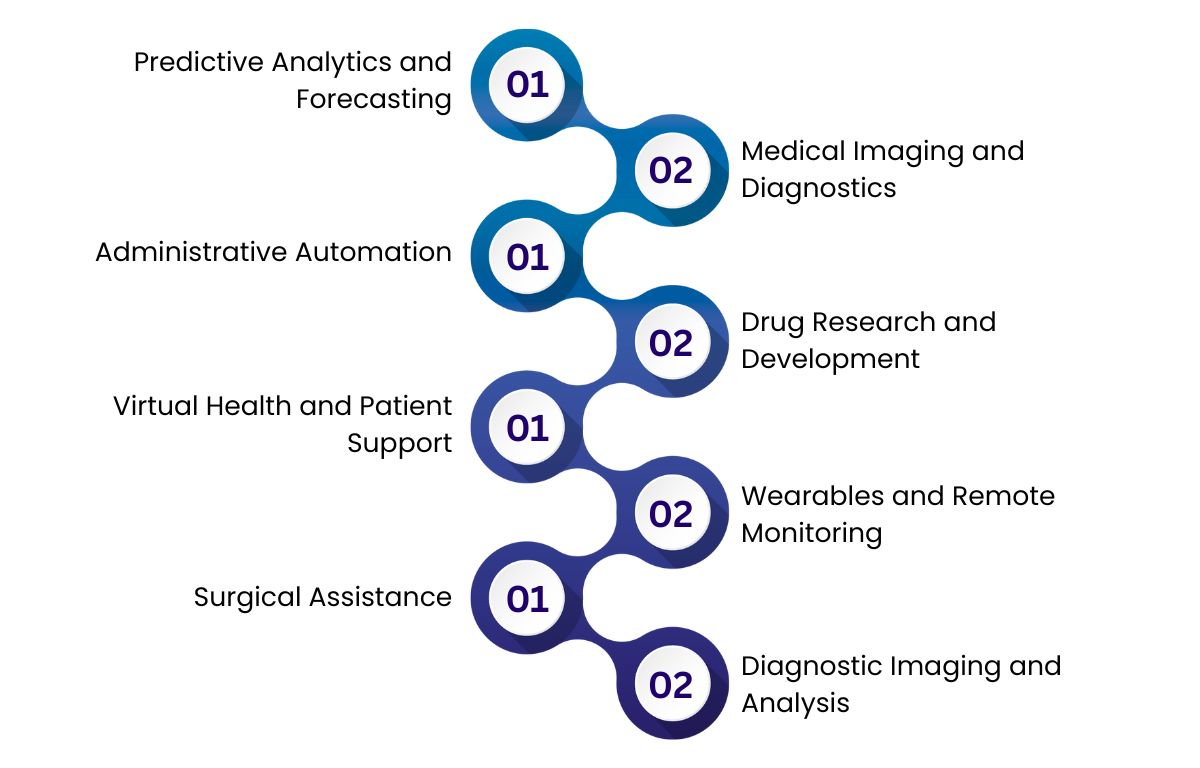
3. Administrative Automation
Billing, insurance claims, staff rosters—most of this work is repetitive. Mistakes cost billions.
An NH hospital that adopted AI-driven billing automation cut claim denials by 55% in a year. That’s revenue back on the table.
And it’s not just money. Staff who once spent hours processing paperwork were freed for higher-value work.
4. Drug Research and Development
Traditional drug discovery takes about 10–12 years.
Cost? Roughly $1.3 billion per drug.
AI shortens preclinical timeframes by predicting molecular interactions and narrowing candidates faster.
Pfizer’s rapid COVID-19 vaccine progress wasn’t just good luck; AI helped process medical literature and datasets at lightning speed.
5. Virtual Health and Patient Support
From appointment scheduling to medication reminders, AI-driven chat systems reduce patient drop-offs and confusion.
Think of them as intelligent assistants, available 24/7, which patients trust more than being stuck on hold.
6. Wearables and Remote Monitoring
Patients with chronic illnesses now wear devices that stream continuous health data to doctors. AI interprets the noise, flags anomalies, and alerts caregivers of potential crises before they escalate.
Early pilots of AI-driven cardiac monitoring reduced rehospitalizations by nearly 38%.
This means fewer emergency events—and lower costs for insurers.
7. Surgical Assistance
AI-assisted robotic surgery isn’t science fiction anymore. Hospitals are already using robotic arms guided by AI software to make precise, stable movements. It’s not robots cutting people open—it’s enhanced precision under human supervision.
The benefits? Faster recovery, fewer errors, less trauma.
8. Diagnostic Imaging and Analysis
Medical imaging is where AI has made the biggest mark. Radiology departments use AI-powered systems to review X-rays, MRIs, and CT scans faster and often more accurately than humans.
For example, AI can spot pneumonia on chest X-rays better than radiologists working alone. These tools reduce diagnostic errors by 20-30%, speed up workflows, and prioritize urgent cases.
With over half of AI medical devices approved in the US and Europe dedicated to radiological applications, this use case is a clear leader.
Want to harness the real potential of AI for your business?
At Zenesys, we create intelligent, secure, and scalable AI solutions that solve real-world challenges.
Explore AI SolutionsWhat is the benefit of using AI in healthcare?
It gives time back.
Time for doctors. Time for patients. Time for families who no longer wait hours for a rushed 10-minute consult.
But that’s not all. Let’s break the benefits down further:
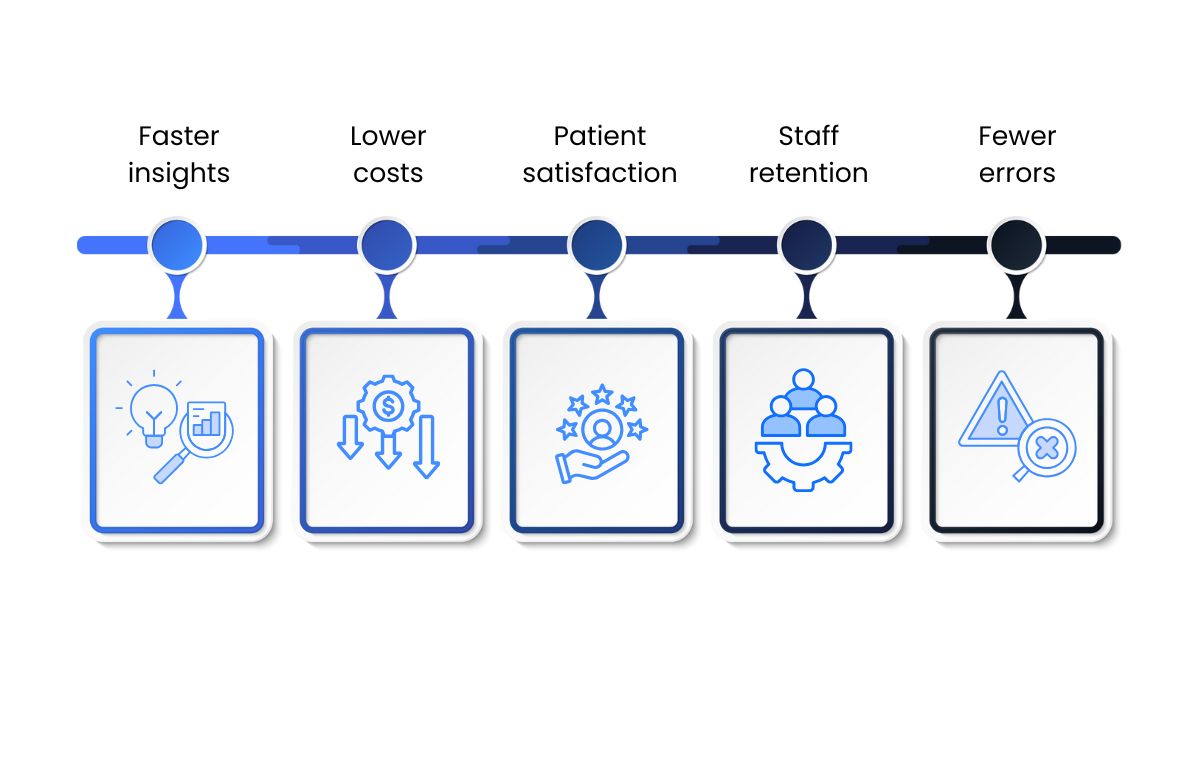
- Faster insights: Diagnosis in minutes instead of weeks.
- Lower costs: Billions saved by AI insurance and billing work.
- Patient satisfaction: Better interactions and more personalized care.
- Staff retention: Less burnout thanks to lighter workloads.
- Fewer errors: Consistency in diagnostic accuracy.
Healthcare is one of the riskiest places for mistakes—because mistakes cost lives. AI directly addresses this.
And the ripple effect is deeper. Lower errors mean fewer lawsuits. More efficient billing means higher cash flow. Patients who feel cared for come back, boosting long-term trust.
AI Agents: From Background to Frontline
Now, let’s talk about AI agents—the “living” applications of AI that interact directly with humans and processes. These aren’t background tools. They’re frontline teammates.
- Patient agents: Virtual nurses, WhatsApp chatbots, voice bots that check in daily on chronic illness patients. They can flag early symptoms that trigger intervention.
- Hospital agents: Staff-scheduling systems that redistribute shifts dynamically. Bed-allocation AI that prevents overcrowding. Discharge agents that ensure patients don’t wait hours for release forms.
- Billing agents: Tools that instantly validate insurance eligibility before care begins—avoiding the nightmare of denied claims later.
Startups around the world are even developing AI care companions—agents that can talk to patients about medication, mental health, and physical exercise, reducing loneliness in elderly populations.
Some health systems are building solutions by hiring an AI company to create secure AI-powered health apps, ensuring patients can interact easily on their smartphones.
The key? AI agents don’t replace doctors or nurses. They extend their reach.
Alho the Healthcare is global, and patients often speak different languages because they could be from different region. Multilingual agents can converse fluently across English, Spanish, Hindi, Mandarin, Arabic, and beyond—removing communication barriers that traditionally slow down care.
AI Governance in Healthcare
This is where responsibility enters. Because with great power, there’s an equally great risk.
AI in healthcare cannot run unchecked. It must be governed with strict rules on fairness, transparency, and safety.
Here are the critical pillars of governance:
Bias and Fairness
AI fed with biased data risks discriminating against minority groups. For example, historically fewer clinical trials include women or minority populations. An AI uncorrected for bias could underdiagnose them.
Governance means rigorous testing, audits, and transparency logs to ensure fairness in all AI recommendations.
Compliance with Laws (HIPAA, GDPR, HITRUST Certification)
Patient data is sacred. AI solutions must encrypt data, prevent unauthorized sharing, and stay compliant with privacy laws. HIPAA in the US and GDPR in Europe are non-negotiable, with heavy fines for violations.
Explainability and Transparency
Doctors won’t adopt AI they don’t understand. A recommendation that says “Patient X: Surgery needed” without reasoning is unusable.
Explainable AI means showing the why behind every prediction.
How to Bring AI Into Healthcare Safely
Hospitals often fail at AI adoption because they treat it as a giant tech project instead of a stepwise process.
Here’s the smarter approach:
- Diagnose the Admin Pain Point First.
Don’t jump to flashy AI tools or robots. Begin where your hospital struggles the most—usually billing errors or chaotic scheduling. Fixing these basics creates the strongest foundation for AI success. - Start Small, Scale Fast.
Pilot one AI tool in just one department. Track its impact carefully. Once you see results, roll it out to other areas. This gradual approach reduces risks and builds confidence. - Set Success Metrics Early.
Know what success looks like from the start. For example, aim to cut denied insurance claims by 20% in three months or reduce ER wait times by 15%. Clear goals keep teams focused and accountable. - Embed Governance.
AI must follow rules. From data privacy to fairness, governance isn’t optional—it’s essential. Include compliance officers and make AI decisions explainable so staff trust the system. - Train Teams.
Doctors and nurses need proper training. Workshops and hands-on support help ease fears about AI replacing jobs. Shift the mindset to AI as a tool that supports, not replaces, their work. - Expand Iteratively.
Once administrative AI tools prove their value, move to diagnostics. Next, bring AI into patient engagement. This step-by-step scaling avoids overwhelm and builds long-term success.
This approach makes AI adoption practical, less risky, and more likely to improve healthcare delivery.
Challenges and Risks No One Should Ignore
- Bias: Left unchecked, AI could make healthcare more unequal.
- Dependency: Doctors over-trusting AI may lose clinical judgment.
- Cybersecurity: Hacking hospital AI means hacking sensitive patient health data.
- Cost: Smaller practices still face high barriers for adoption, both technology and training.
- Mistrust: Many patients remain skeptical. A survey found 60% of patients prefer human-only diagnosis even if AI is statistically more accurate.
Why Zenesys Could Be Your Partner in AI-Powered Healthcare
Adopting AI in healthcare isn’t just about installing software. It’s about designing solutions that meet strict compliance standards, protect sensitive data, and actually improve patient outcomes. That takes expertise in both technology and healthcare.
That’s where Zenesys Solutions Inc. comes in.
We’ve been helping healthcare organizations adopt digital solutions for years—projects that range from secure patient portals and electronic health record (EHR) systems to AI-powered analytics dashboards. Our teams have worked on projects that involve:
- AI-driven patient engagement tools that improve communication between providers and patients.
- Healthcare analytics platforms that use machine learning to predict patient outcomes and reduce readmission rates.
- HIPAA-compliant web and mobile applications designed for hospitals and clinics, ensuring data privacy isn’t compromised.
- Integration of AI with IoT devices like wearables, enabling remote monitoring and early detection of health risks.
We don’t just build apps—we build healthcare-ready AI systems that balance speed, accuracy, and compliance.
Here’s the advantage: when you partner with Zenesys, you’re not just getting coders. You’re getting a team that understands the nuances of healthcare regulations, patient data sensitivity, and the urgency of building solutions that actually work in real-world hospital environments.
Sounds ambitious? Yes. But it’s exactly what healthcare providers need right now.
If your organization is considering AI adoption—whether it’s smarter patient portals, AI predictive analytics, or even AI-powered diagnostic tools—Zenesys could be your partner in making it real.
Conclusion
The question isn’t if hospitals will adopt AI. The question is how fast and how well.
Here’s the window: in 3–5 years, AI-powered diagnostics, billing automation, and patient bots won’t be “new.” They will be expected.
Think about banking. Remember when mobile apps were optional? Today, if a bank doesn’t have one, it looks outdated. That’s where healthcare is heading with AI.
Hospitals acting now will set the standards. They’ll cut costs, retain staff, and win patient loyalty before others catch up.
Hospitals waiting it out? They’ll struggle to survive.
The choice is brutal but simple. Start small. Build trust. Govern smartly. Scale steadily.
Because in healthcare, hesitation doesn’t just cost market share—it costs lives.


.webp?lang=en-US&ext=.webp)

.webp?lang=en-US&ext=.webp)